Il sintomo principale dei pazienti critici, quelli di tipo C, è l’insufficienza respiratoria.
Cerchiamo di capire meglio di cosa si tratta. Più sappiamo e più siamo in grado di difenderci dalla minaccia.
Come inizia
La mancanza di respiro, o insufficienza respiratoria, causata dal Coronavirus, è una forma di polmonite.
Il virus si replica e si diffonde nell’apparato respiratorio e inizia a danneggiare le cellule del polmone.
A questo punto il nostro sistema immunitario si attiva, come un esercito, e genera una forte risposta di difesa! Il nostro corpo però non è ben preparato al nemico, come un esercito che non conosce bene l’invasore e quindi avvia una risposta generica e non focalizzata.

Questa è l’infiammazione: arrivano i globuli bianchi con tutto un contorno di armi generiche, pronti a combattere; si fa spazio all’arrivo delle truppe, si allargano le autostrade (vasi sanguigni) per fare spazio ai camion con soldati freschi in arrivo. E inizia la battaglia all’arma bianca.
Conseguenze
Sul campo di battaglia, che è il polmone, rimangono a terra man mano le truppe colpite. I globuli bianchi vengono rimpiazzati da altri globuli bianchi, arrivano altre truppe. Un po’ alla volta si accumula del materiale negli spazi tra le cellule del polmone che sono dedicate a processare l’Ossigeno e gli altri gas respiratori.
In altre parole, succede quello che accade quando ci facciamo un ematoma su un braccio: SI GONFIA TUTTO PER 15 GIORNI!
Cerchiamo di visualizzare il problema con delle immagini.
Questa che state per vedere è una immagine di un polmone normalmente areato, dove l’aria che viene scambiata per respirare è indicata in grigio scuro.
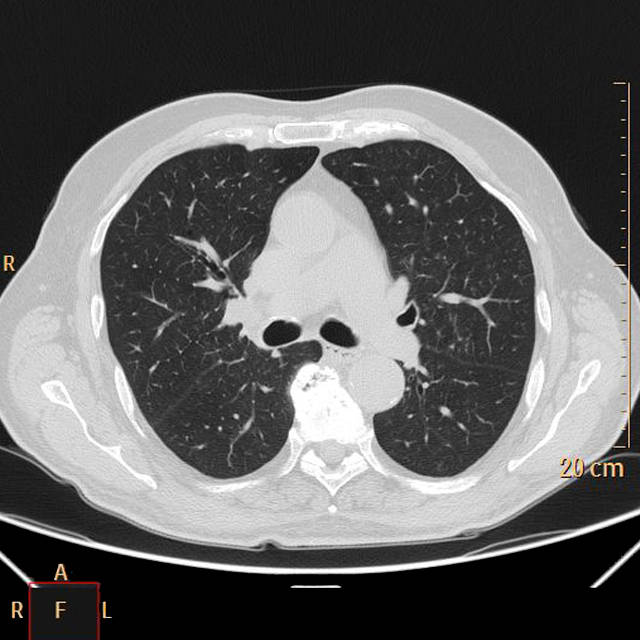
Questa qui sotto invece è l’immagine tratta da un paziente con polmonite da Coronavirus: come potete vedere l’aria grigia presente nel polmone è molto poca, perchè viene sostituita da tutte le cellule infiammatorie, detriti etc che “compattano” il polmone (parte bianca) e non consentono un ingresso e una diffusione dell’aria sufficiente per permettere all’individuo di ottenere abbastanza ossigeno.
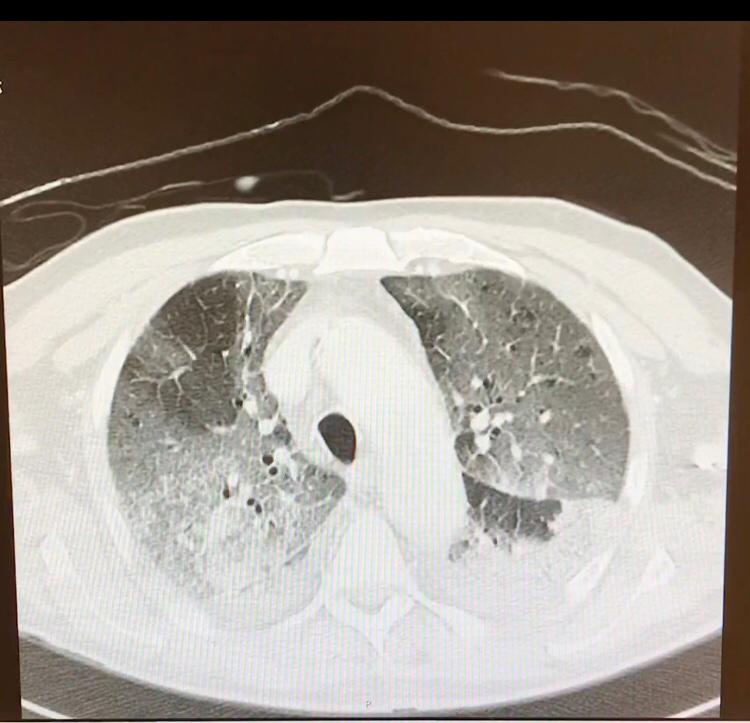
Cosa accade dunque? Che la quantità di Ossigeno che riesce ad entrare nel polmone è troppo esigua e la persona percepisce un senso di “fame d’aria” e non riesce più a respirare.
Rispetto agli altri pazienti con polmonite, inoltre, “il paziente con Coronavirus arriva alla fatica dei muscoli respiratori più tardi del tipico paziente con ARDS e bassa compliance: è falsamente tranquillizzante, ma può progredire subdolamente verso un peggioramento drammatico non anticipato da una grave dispnea a riposo” (1).
Probabilmente i casi di sincope che abbiamo osservato nei video cinesi sono dovuti al fenomeno descritto sopra; pare infatti che questi malati, rispetto agli altri malati di polmonite, abbiano una maggiore tendenza all’abbassamento dei livelli di ossigeno nel sangue (1).
Trattamento
I pazienti critici vengono trattati in terapia intensiva.
Ventilazione non invasiva
Alcuni pazienti critici riescono a trarre beneficio da un aiuto alla ventilazione non invasivo, con dei caschi o delle maschere che aderiscono alla faccia e collegate ad un ventilatore che aiuta il paziente spingere l’aria nei polmoni ad ogni atto respiratorio. Tuttavia nel caso della polmonite da Coronavirus questo tipo di ventilazione pare sconsigliabile perchè:
- molti pazienti devono successivamente essere sottoposti comunque a ventilazione meccanica invasiva;
- durante la ventilazione non invasiva l’aria (e quindi il virus) esce dal paziente e può infettare comunque
- il paziente richiede comunque l’uso di un ventilatore che non può essere destinato ad altri pazenti.
Ventilazione invasiva (o meccanica)
Il trattamento più efficace dei pazienti critici con insufficienza respiratoria acuta da Coronavirus dunque è la ventilazione meccanica. Il polmone di questi soggetti diventa pieno di detriti e “rigido”, per cui la ventilazione non è efficace. Il senso della ventilazione meccanica ai pazienti con polmonite da coronavirus consiste nel riuscire a garantire l’adeguata ossigenazione in attesa che il quadro di infezione/infiammazione man mano si riduca.
Sembra che la ventilazione meccanica precoce sia più efficace a garantire l’ossigenazione dei tessuti e sia legata in qualche modo ad un potenziale migliore outcome, ma ovviamente è presto per affermarlo con certezza.
Qualora non fosse sufficiente la ventilazione meccanica a volte è disponibile anche un trattamento “eroico”, che consiste nell’utilizzo di una macchina che preleva il sangue dal paziente, lo ossigena esternamente al paziente e poi lo reinfonde (ECMO).
Le tecniche di rianimazione avanzata che vi abbiamo raccontato sono disponibili solo nelle terapie intensive. Ecco perchè è fondamentale potenziarle nell’ottica di poter garantire il trattamento più efficace per il maggior numero di malati critici possibile.
Quanti letti per i pazienti critici potrebbero servire? Leggete le previsioni giorno per giorno fatte con la nostra matematica: e’ l’ora di reagire!
Come si stanno organizzando gli ospedali in risposta all’aumento dei pazienti critici?

Dott. Marco De Nardin
(1) http://www.ventilab.org/2020/02/29/ventilazione-meccanica-e-polmonite-da-coronavirus/