L’emergenza Coronavirus ha determinato una riorganizzazione degli ospedali e in particolare degli sconvolgimenti nella struttura, logistica e gestione dei reparti di terapia intensiva. Oggi ci occupiamo di come sono state strutturate le terapie intensive degli ospedali Covid-19.
L’aumento repentino della necessità
Quando si è sviluppata l’emergenza Covid-19 il numero dei pazienti critici è aumentato improvvisamente ed è stato necessario decidere dove posizionare i pazienti critici che man mano si accumulavano. In un primo momento i posti letto occupati per primi erano quelli disponibili nelle terapie intensive esistenti. In un secondo tempo, anche nell’ottica di separare i pazienti covid-19 da quelli non-covid, è stato necessario dedicare delle terapie intensive esclusivamente a pazienti covid.
Terapie intensive “dedicate” covid-19
Sono state perciò identificate, a tavolino, delle terapie intensive che avrebbero alloggiato solo pazienti covid-19. Man mano che queste si riempivano di pazienti è emersa la necessità di potenziare i posti letto di queste terapie intensive dedicate. La struttura dei reparti spesso è limitata logisticamente (pareti, prese di ossigeno eccetera), per cui nella maggior parte dei casi non è stato possibile aumentare i posti letto nelle terapie intensive esistenti. Di conseguenza bisognava dedicare altre aree ospedaliere, usualmente destinate ad altro utilizzo, come terapie intensive aggiuntive.
Creazione di nuove strutture dedicate covid-19
Da 1 terapia intensiva con 4-6 o 8 letti si è passati, negli ospedali che venivano dedicati al Covid-19, a 2 o 3 o 4 terapie intensive. Quindi da una media di 6-8 letti si è passati a 24, 30, anche 40 letti! Dove sono state ricavate queste strutture?
Strutture esistenti
In alcune situazioni sono stati modificati gli usi delle strutture esistenti: per esempio la terapia intensiva dedicata ai pazienti cardiochirurgici è stata dedicata ad alloggiare pazienti covid. In questo caso non sono state fatte modifiche di nessun tipo alla struttura ma è cambiata solo la tipologia dei pazienti.
Sale operatorie
Dopo aver occupato tutte le terapie intensive disponibili sono state allestite le sale operatorie: invece di fare interventi chirurgici, sospesi definitivamente, in questi ospedali ogni sala operatoria si è trasformata in una terapia intensiva. Al posto dei macchinari di sala operatoria ecco entrare i letti di terapia intensiva. In ogni sala sono stati ricavati da 2 a 4 letti con l’aggiunta di ventilatori, macchine per dialisi, pompe di infusione, tutto il necessario per creare un posto letto di terapia intensiva in sala operatoria.
In alcuni ospedali dove le sale operatorie sono dotate di una sala di risveglio dei pazienti molto attrezzata, anche con i ventilatori, questa sala risveglio è diventata sala di rianimazione.
Strutture nuove
In altri casi ancora, dove non erano sufficienti anche le sale operatorie, si è deciso di creare delle terapie intensive ad hoc. Il sistema sanitario ha creato delle strutture dedicate, adibite ad accogliere le degenze intensive. È stato portato tutto il materiale in fretta e furia e si è allestito un intero reparto: una procedura che in genere richiede mesi si è svolta in una settimana o poco più. A volte si sono posizionati i monitor sull’incavo delle finestre anziché sui classici pensili: gli ambienti sono stati adattati alle necessità.
La logistica dei locali
In tutto questo gran subbuglio vogliamo raccontare come è cambiata l’attività degli operatori sanitari a livello logistico. La prima cosa da conoscere in questo senso è la differenza tra terapie intensive “a stanzone unico” e quelle “a box chiusi” o isolati.
Terapie intensive “a stanzone unico”
Le terapie intensive “a stanzone unico” sono dei locali grandi e unici in cui tutti i malati e gli operatori si trovano nella stessa grande stanza. Anche le postazioni con i computer etc sono nel medesimo grande ambiente. In questo tipo di locale il virus ovviamente è diffuso ovunque. Gli operatori lavorano tutto il tempo con il massimo delle protezioni addosso.
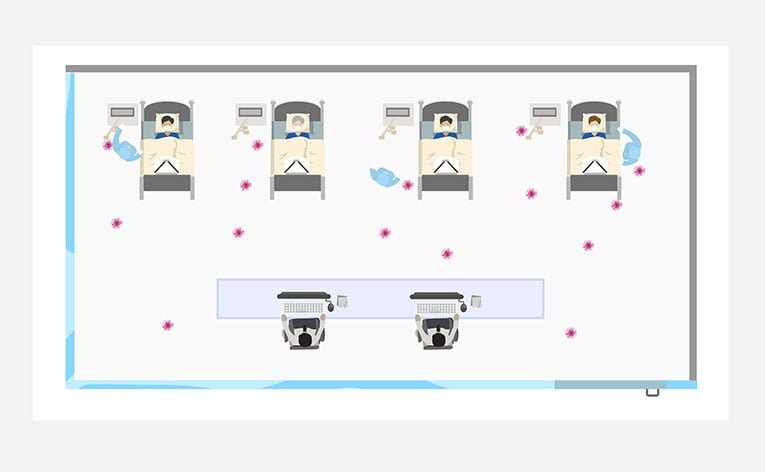
Vantaggi:
- Tutte le comunicazioni tra gli operatori sono immediate: si trovano tutti nello stesso ambiente.
- L’ambiente di lavoro unico consente una maggiore “vicinanza” e collaborazione del personale.
- Gli operatori non devono cambiarsi frequentemente. Si risparmia qualche mezzo di protezione individuale.
- Maggiore organizzazione mentale: quando si è al lavoro si sa di essere in un ambiente a rischio, sempre e comunque.
Svantaggi:
- Maggiore difficoltà a fare pausa per il personale con maggiore stanchezza e frustrazione.
- Maggiore difficoltà nel lavorare al computer con doppi guanti, accaldati, con difficoltà acustica significativa.
- Difficoltà di svolgere un dialogo tra il personale che non si limiti a pochi ordini precisi.
Terapie intensive “a box chiusi”
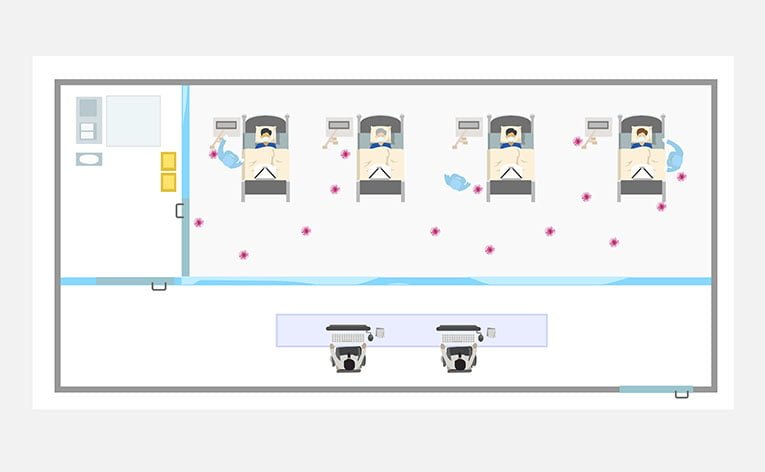
Le terapie intensive “a box chiusi” prevedono dei locali separati: alcuni locali per alloggiare i pazienti infetti e gli operatori che li assistono e altri locali per il personale di supporto che non assiste direttamente i malati o utilizzati nel momento in cui questi ultimi non assistono i malati. Qualcuno si potrebbe meravigliare che l’attività di assistenza non sia la sola o la principale attività di lavoro svolta negli ospedali, ma è la normalità. Basti pensare che i medici svolgono molte attività lontano dai pazienti stessi.
Quali sono queste attività non assistenziali? Tra le tante, citiamo:
- la prescrizione delle terapie;
- la richiesta e la valutazione degli esami di laboratorio e strumentali;
- il dialogo tra colleghi per scegliere le terapie più appropriate per i pazienti.
Tutte queste attività di norma non avvengono nello stesso ambiente dove si trovano i malati.
Il virus è presente nei locali di degenza, ma non nei locali esterni: questo determina diversi vantaggi e svantaggi rispetto al sistema a stanzone unico.
Vantaggi:
- Il personale è in grado di poter alternare le attività assistenziali con attività tecniche o burocratiche in ambienti distinti;
- Il personale è in grado di alternare le attività faticose con quelle meno impegnative sia mentalmente che fisicamente;
- Minore stanchezza e frustrazione durante i turni, possibilità di esecuzione di turni prolungati con maggiore efficienza;
- Maggiore efficienza e concentrazione nell’attività burocratica.
Svantaggi:
- L’ambiente di lavoro unico consente una maggiore “vicinanza” e collaborazione del personale;
- Gli operatori devono cambiarsi più frequentemente. Aumenta l’utilizzo di dispositivi di protezione individuali;
- Maggiore organizzazione mentale: quando si è al lavoro si sa di essere in un ambiente a rischio, sempre e comunque;
- Difficoltà di dialogo tra il personale che assiste i malati e il personale dirigente;
- Necessità di sistemi di comunicazione specifici.
Con questo articolo abbiamo iniziato a scoprire le peculiarità delle terapie intensive covid-19. Continueremo questo viaggio alla scoperta di questa realtà sempre nuova e in evoluzione nei prossimi articoli.