Non solo terapie intensive!
All’inizio dell’epidemia avevamo segnalato come il problema principale, per cui tutti avrebbero dovuto stare in casa, consisteva nel fatto che ci sarebbero stati moltissimi malati critici tutti in contemporanea e che non sarebbe stato possibile trattarli con le risorse attuali.
La quantità di malati critici e di decessi avrebbe determinato diversi scenari di gravità, a seconda dell’applicazione o meno di misure più o meno restrittive messe in atto dalle autorità.
La combinazione delle misure restrittive e l’enorme sforzo di aumento dei posti nelle terapie intensive per i malati critici ha consentito finora di riuscire a gestire l’emergenza senza dover per il momento ricorrere a scegliere quali malati trattare.
Nel frattempo pare che la curva dei contagi sia in appiattimento e questo ci fa ben sperare
Attualmente l’arrivo massiccio di malati nelle terapie intensive, per il momento, con le misure messe in atto, sembra avere retto, se non del tutto in Lombardia, per lo meno nelle altre regioni del Nord Italia.
L’attenzione sui malati “intermedi”
Ora l’attenzione di noi medici in prima linea è concentrata, oltre che su questi pazienti critici, anche sui malati cosiddetti “intermedi”.
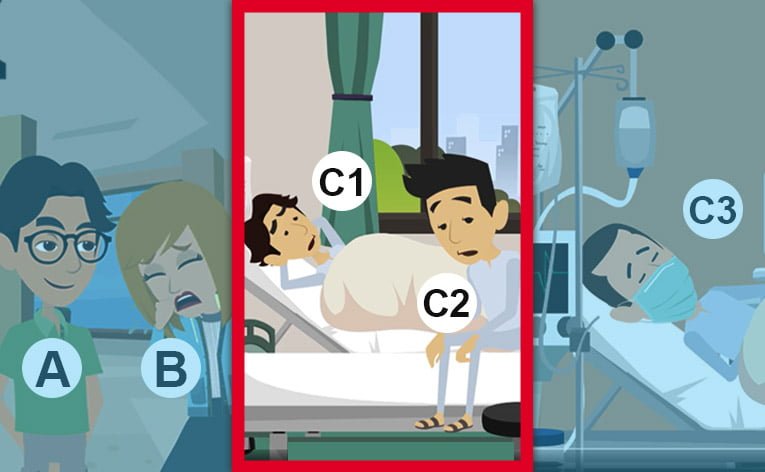
Ricapitoliamo che avevamo identificato i pazienti positivi al Coronavirus in tre diverse categorie o quadri clinici:

- il tipo A, cioè gli asintomatici,
- il tipo B, quello dei malati lievi che possono stare a casa e non richiedono un ricovero ospedaliero, e
- il tipo C, quello dei malati critici, che richiedono un ricovero ospedaliero perchè presentano un’insufficienza respiratoria.
Ora i pazienti con quadro di tipo C possono essere ulteriormente suddivisi in 3 sottogruppi, in base alla loro situazione:

- C1, con mancanza di respiro LIEVE, che richiedono soltanto OSSIGENO
- C2, con mancanza di respiro MODERATA, che richiedono SOSTEGNO VENTILATORIO NON INVASIVO
- C3, MOLTO GRAVI, da terapia intensiva, che richiedono ventilazione invasiva.
I pazienti di tipo C1 e C2 sono appunto quelli che definiamo malati “intermedi”, che sono abbastanza ammalati da stare in ospedale ma non ancora così critici da essere trattati in terapia intensiva.
Questi ammalati attualmente riempiono fette sempre più consistenti dei nostri ospedali. La VERA SFIDA, ora, consiste nel comprendere meglio l’evoluzione della malattia in questi soggetti. La analizziamo sotto tre versanti:
1. La prevenzione
La prima linea di intervento nei confronti dei malati “intermedi” consiste nel cercare di PREVENIRE il peggioramento di questi ammalati verso la fase di criticità che potrebbe condurli in terapia intensiva. Questo potrebbe “alleggerire” le condizioni di salute di questi soggetti, ridurre la mortalità e l’impatto della malattia nei loro confronti. Le terapie sperimentali in corso hanno l’ambizione di “congelare” la malattia ai livelli di sviluppo più precoci, riducendone l’impatto.
2. Identificazione dei segni precoci di peggioramento
In alternativa, si sta cercando di identificare dei “SEGNI PRECOCI” di peggioramento, in modo da anticipare il trasferimento in ambito intensivo di alcuni pazienti e di conoscere in anticipo l’evoluzione positiva degli altri. (1)
3. Modifica dei sistemi di diagnosi
Si sta anche cercando di modificare e snellire i sistemi diagnostici per rendere più rapido il processo decisionale e per evitare di dover trasferire i malati in altri reparti, per esempio in radiologia, con grossi rischi di infezione tra pazienti e personale.
Conclusioni
Tra le tante situazioni aperte nell’emergenza Coronavirus una di esse è costituita dalla gestione di quei malati “intermedi” che non sono così critici da richiedere la terapia intensiva, ma lo possono rapidamente diventare. La nuova sfida è stata appena lanciata e i nuovi approcci diagnostici, terapeutici e di prevenzione ci aiuteranno a ridurre l’impatto della malattia su questi soggetti e sul sistema sanitario.
NOTE
(1) Per esempio in quest’ottica pare che fare un’ecografia polmonare possa fare aiutare a distinguere i pazienti con sindrome interstiziale “wet” (bagnato), cioè solo linee B ed uno sliding conservato dai pazienti “dry” (secco), con una sindrome interstiziale composta da multipli consolidamenti sub-pleurici e sliding ridotto. Nel primo caso si può pensare ad un tentativo con ventilazione non invasiva (C-PAP o NIV), mentre nel secondo è necessaria l’intubazione precoce.

Dott. Marco De Nardin