I tamponi faringei sono davvero efficaci per la diagnosi di Coronavirus?
In questo articolo analizziamo se i tamponi faringei siano davvero efficaci ed affidabili per determinare la diagnosi di Coronavirus, cioè per stabilire se una persona sia positiva o meno al Coronavirus.
ATTENZIONE: Le informazioni che si trovano qui riguardano i tamponi MOLECOLARI. Per ulteriori informazioni sui tamponi RAPIDI rimandiamo al seguente articolo:
Questo argomento è particolarmente attuale, dal momento che è stato istituito l’obbligo di tampone per molti nostri connazionali che rientrano dall’estero all’Italia.
Come già visto in maniera più approfondita in altri articoli, quando è necessario verificare se un paziente sia infetto dal Coronavirus attualmente viene eseguito un test diagnostico specifico su un campione biologico. Di solito questo campione consiste in una piccola quantità di muco prelevata dal naso (tampone nasale) o dalla gola (tampone faringeo). Quando possibile, possono essere prelevati dei campioni di espettorato o broncolavaggio dalle vie respiratorie profonde, ma sono molto meno comuni e più laboriosi da ottenere e si eseguono in specifiche circostanze.
Dall’inizio dell’epidemia ad oggi, i tamponi nasali e faringei sono sicuramente stati i campioni più prelevati, per screening e per diagnosticare la presenza del virus, grazie all’accessibilità delle vie aeree superiori e alla facilità di esecuzione del prelievo.
I campioni di muco dei malati sono tutti positivi?
In una situazione in cui questi test diagnostici sono così largamente utilizzati per identificare le persone infette all’interno della popolazione, è importante considerare i loro limiti. Quale certezza abbiamo di intercettare il virus nei campioni di muco delle persone infette da Covid-19 all’interno dei campioni nasali o faringei? Se i test eseguiti su questi campioni dessero un alto numero di falsi negativi, cioè di risultati negativi nonostante le persone siano malate, questo vuol dire che una parte consistente di popolazione infetta, e quindi contagiosa, potrebbe essere sfuggita ai radar e aver contribuito silenziosamente alla diffusione del contagio. Per chi non ricordi cosa è un falso negativo vi rimandiamo alla lettura di un nostro articolo in cui viene spiegato questo concetto, relativamente alla misurazione della temperatura corporea come metodo per evidenziare l’infezione.
Le impressioni cliniche
Quando abbiamo iniziato a richiedere i primi tamponi eravamo trepidanti, in attesa del risultato, per capire se il paziente con cui avevamo avuto contatto era o meno positivo.
Avevamo grande fiducia nel fatto che il tampone potesse darci delle informazioni esaustive.
Man mano che passava il tempo, però, si sono intensificati i casi di pazienti che venivano in ospedale con febbre o difficoltà respiratoria a cui veniva eseguito un tampone con esito negativo, anche più di uno. A distanza di giorni e dopo un peggioramento delle condizioni cliniche questi pazienti presentavano la positività al tampone! Anche dopo uno, due, tre o quattro tamponi negativi!
Abbiamo perciò incominciato a chiederci: non sarà mica che il tampone ha una bassa probabilità di individuare i soggetti positivi? Del resto abbiamo già sottolineato nel nostro articolo sui test per i tamponi che se è positivo non vi sia un grande errore (1). Poco invece ancora si conosce sulla effettiva capacità del test di individuare coloro che hanno il Coronavirus.
Come capire se i tamponi faringei sono affidabili per la diagnosi di Coronavirus?
Si è cominciato perciò a studiare il fenomeno. Come si può fare? Beh, allora per capire se il test applicato ai tamponi è in grado di identificare qualcosa, bisogna prima stabilire un metodo per identificare quel qualcosa che si deve identificare.
In altri termini: quando ci si chiede se un metodo è efficace consiste nel confrontarlo con un altro metodo. Il problema però è: esiste un altro metodo con cui confrontare il test del tampone? Sfortunatamente la risposta è NO. Il test del tampone è attualmente l’unico metodo utile per identificare i pazienti con il Coronavirus.
Già da questo fatto si comprende come la faccenda sia piuttosto intricata. Perché non esiste un altro metodo, quello che noi in medicina chiamiamo “gold standard”, col quale confrontare il test del tampone.
L’unico metodo disponibile per confermare l’efficacia del test del tampone è verificarlo in pazienti QUASI CERTAMENTE POSITIVI perché ammalati di Covid-19 in modo inequivocabile. Solo i pazienti con DIAGNOSI CLINICA di Covid-19 corrispondono infatti ad un buon gruppo di confronto per valutare il test del tampone.
Per capire meglio cosa si intende per affidabilità di un test diagnostico rimandiamo all’articolo: Affidabilità di un test diagnostico: matematica e teorema di Bayes
Lo studio
Una prima risposta parziale ci deriva da uno studio pilota condotto in Cina su 205 pazienti con diagnosi di Covid. Nello studio la diagnosi di Covid-19 veniva eseguita tramite la presenza di:
- sintomi tipici della malattia (febbre, tosse secca e affaticamento);
- esami radiologici (positivitità per polmonite a Rx torace o TAC);
- rilevamento di Coronavirus CoV2 in un campione biologico.
In questi pazienti sono stati esaminati vari campioni biologici a tappeto. È stata fatta una ricerca del Coronavirus nei vari fluidi o escrezioni corporee per capire dove è più frequente trovare il Coronavirus.
Durante lo studio i medici hanno quindi prelevato da questi pazienti, sei diversi tipi di campioni biologici oltre a quelli normalmente prelevati durante un tampone naso-faringeo, e in vari momenti durante il corso della malattia.
In totale i campioni comprendevano 1070 prelievi tra sangue, feci, urine e anche materiale espulso dalle vie respiratorie profonde (detto “espettorato”). Per i pazienti più gravi, sottoposti alla ventilazione meccanica poiché non più capaci di respirare da soli, erano anche disponibili campioni di broncolavaggio e biopsie, cioè piccoli campioni, di tessuto delle vie respiratorie.
Ebbene, gli studiosi hanno eseguito il test diagnostico per rilevare la presenza di SARS-CoV-2 in tutti i campioni, cercando di rilevare il materiale genetico del virus. Idealmente, la maggioranza dei campioni sarebbe dovuta risultare positiva, perlomeno provenienti dalle vie respiratorie dove normalmente si annida il virus.
I RISULTATI: i campioni prelevati da naso e gola non sono così attendibili come pensavamo
I risultati dello studio (riportati in tabella) sono stati piuttosto inaspettati.
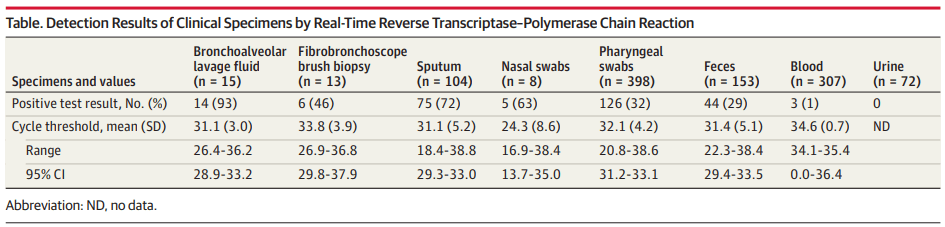
Sono stati analizzati campioni provenienti da:
- Broncolavaggio: 15 campioni, 14 positivi, Attendibilità (2): 93%
- Biopsia con broncoscopia: 13 campioni, 6 positivi, Attendibilità (2): 46%
- Espettorato (sputum): 104 campioni, 14 positivi, Attendibilità (2): 72%
- Tampone nasale: 8 campioni, 5 positivi, Attendibilità (2): 63%
- Tampone faringeo: 398 campioni, 126 positivi, Attendibilità (2): 32%
- Feci: 153 campioni, 44 positivi, Attendibilità (2): 29%
- Sangue: 307 campioni, 3 positivi, Attendibilità (2): 1%
- Urine: 72 campioni, 0 positivi, Attendibilità (2): 0%
Analisi dei dati ottenuti
Solo il 32% dei TAMPONI FARINGEI di persone infette risultano positivi, lasciando 2/3 dei casi non diagnosticati correttamente. La conferma di questi dati potrebbe avere importanti conseguenze sul conteggio dei casi reali in Italia e nel resto del mondo, nonché sulle strategie di contenimento del contagio.
Il virus è presente in maniera non trascurabile nelle FECI dei soggetti. Ecco quindi la conferma del riscontro di alcuni casi di trasmissione orofecale. Ricolleghiamo questo dato anche alla presenza di DIARREA come sintomo premonitore di Coronavirus.
Le cose si sono ulteriormente complicate quando gli studiosi hanno notato che, nonostante la malattia sia conclamata, non tutti i campioni biologici provenienti dallo stesso paziente risultano positivi. Per una persona magari erano positivi l’espettorato, ma non le feci o il tampone faringeo; per un’altra invece avveniva il contrario, con tampone faringeo positivo e feci ed espettorato privi di materiale genetico incriminato.
Conclusione: i tamponi faringei sono efficaci per la diagnosi di Coronavirus?
Complessivamente che cosa ci dicono queste informazioni? Ci indicano che la diagnosi dai soli campioni nasali o faringei potrebbe non essere attendibile perché risulta errata rispettivamente in 1/3 e 2/3 dei casi. Per minimizzare il più possibile i risultati degli esami falsamente positivi, cioè quelli che non indicano che il paziente è infetto quando invece lo è, sarebbe utile eseguire il test su campioni delle vie respiratorie inferiori, che sembrano essere più attendibili. Tuttavia il metodo non è certamente applicabile su larga scala. Inoltre, una buona strategia potrebbe prevedere di eseguire il test su più campioni dello stesso paziente, per diminuire la probabilità di errore e quindi essere più sicuri del risultato negativo.
Se ti è piaciuto questo articolo e vuoi rimanere aggiornato sulle nostre prossime pubblicazioni clicca qui per iscriverti alla nostra newsletter.
Note
- (1) la specificità è molto elevata, per lo meno secondo i risultati che abbiamo potuto trovare in rete: https://www.med4.care/coronavirus-il-test-diagnostico/
- (2) per Attendibilità ci si riferisce alla Sensibilità. Si è usato questo termine per consentire a tutti di comprendere il significato “comune” del termine
Referenze:
- Wang W, Xu Y, Gao R, et al (2020) Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA https://doi.org/10.1001/jama.2020.3786, https://jamanetwork.com/journals/jama/fullarticle/2762997?resultClick=1